What is Pigmented Villonodular Synovitis?
Pigmented Villonodular Synovitis (PVNS) is a benign (non-cancerous) condition that occurs due to overgrowth of the synovium, the tissues that line the joints, or production of excess synovial fluid. PVNS can be localized, where only a portion of the joint is affected, or diffused, where the condition is more widespread and involves the entire joint. While PVNS can affect any joint, it most commonly affects the knee and presents with pain, swelling, and stiffness. Without treatment, it can continue to grow and cause arthritis, tendon or joint damage.
Who is usually affected?
- • The majority of cases occur in adults between the ages of 30s-40s, however it can occur at any age.
- • Rare in children.
- • Equally as common in males and females.
Common Sites Involved
- • PVNS occurs in the joint synovium:
- • Knee (most common site)
- • Hip
- • Ankle
- • Shoulder
- • Elbow
Causes
- • The cause of PVNS is unknown.
Biological Behavior
- • Aggressive proliferation of cells in the synovium.
- • Tumor destroys cartilage, which can result in arthritis in severe cases.
- • Bursa frequently involved.
Signs and Symptoms
- • Signs and symptoms include a slow growing mass, gradual pain and swelling, decreased range of motion, and the affected area may be sensitive to palpation or touch.
- • Patients with cases of local PVNS present with pain, catching, locking, and instability of the affected area.
- • In long-standing cases there may be destruction of cartilage, secondary degenerative change, and pain characteristically in diffuse PVNS.
Diagnosis
- • The work-up for PVNS often consists of a physical examination, X-ray, MRI, CT, and bone scans. The diagnosis is often confirmed with a synovial biopsy, which samples the tumor for further analysis. The sample synovial fluid will appear brown, due to old blood, if positive for PVNS.
- • Synovial fluid aspiration is a very common way to promptly diagnose this tumor.
Risk to your limbs
Pigmented Villonodular Synovitis (PVNS) is a non-cancerous condition that occurs due to overgrowth of the synovium, the tissues that line the joints, or production of excess synovial fluid. The risks associated with PVNS include invasion and destruction of the neighboring bone, destruction of cartilage, extension beyond the joint into adjacent nearby tissue, arthritis, and in very rare circumstances can become malignant.
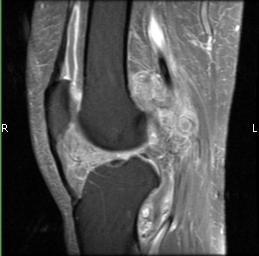
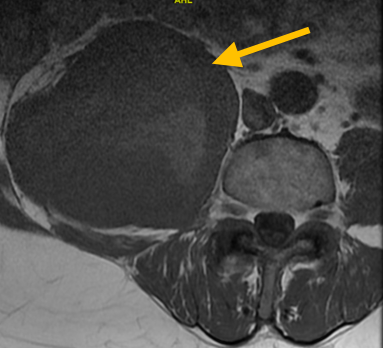
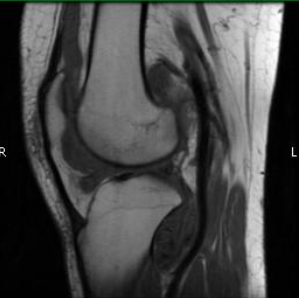
Radiographic imaging is used to help form a diagnosis of PVNS. These include X-Ray, MRI, CT and Bone Scans.
An example of an MRI is shown.
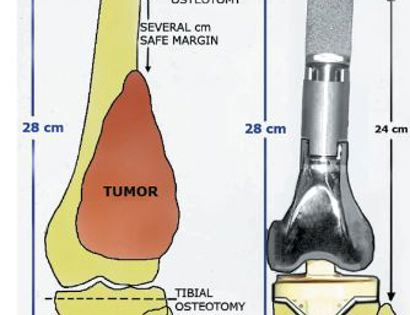
Treatment of Pigmented Villonodular Synovitis
The treatment of pigmented villonodular synovitis (PVNS) varies depending on the location and severity of the condition. Treatment options typically include open synovectomy, arthroscopic synovectomy, combined arthroscopic/open synovectomy, and joint excision/replacement. Specifically, for diffuse PVNS which is associated with high recurrence rates, treatment includes an open synovectomy. There are more limited treatment options for local PVNS, however an arthroscopy partial synovectomy may be performed. Radiation may also be considered in conjunction with surgery, which can help with local control.
Synovectomy
An open synovectomy is a surgical procedure, in which an incision is made to the affected joint and the excess synovium causing PVNS is surgically removed. On the other hand, an arthroscopic synovectomy is a minimally invasive surgery which uses an arthroscope and makes small incisions to remove the excess synovium. Synovectomies are procedures to treat PVNS and can be performed as an open synovectomy, arthroscopic synovectomy, or combination of both.
Radiation
Radiation is a treatment option for some cancers. Radiation therapy is a localized treatment that utilizes high-energy particles or waves to kill cancerous cells. Because radiation therapy is a localized treatment, it only affects the area in which it is set to target and therefore eliminates the risks of damaging healthy cells throughout the body. Not only is it used to treat cancer, but it can also decrease the chances of the cancer from recurring. Lastly, radiation may be used in conjunction with other treatments, such as surgery or chemotherapy, to treat cancers.
Joint Replacement