What is a Limb-Sparing Surgery of the Lower Leg/Knee?
The knee joint consists of your femur, tibia, fibula, and patella. The distal (lower portion) femur and its diaphysis (middle portion) are common sites for primary bone sarcomas and metastatic tumors. Some of these tumors include osteosarcomas, chondrosarcomas, and ewing’s sarcomas. Limb-sparing surgery can be performed for approximately 95% of tumors arising from the lower femur. In some instances, the extremity cannot be saved and an amputation is performed.
Contraindications for saving the limb may include neurovascular invasion, infection, pathological fracture, extensive disease, contamination from a poorly performed biopsy, recurrent disease.
What’s involved in the technique?
Incision
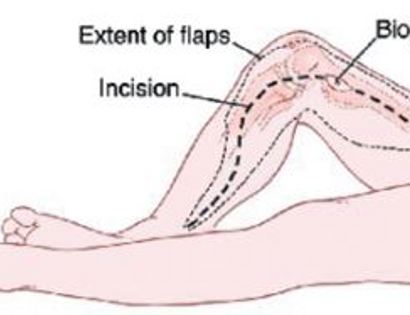
A long incision is made from the upper thigh to the upper tibial bone.
Muscle Releases
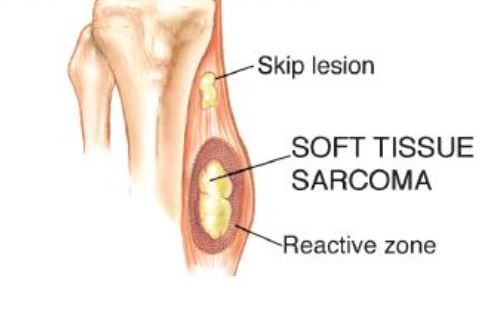
Developing surgical planes (margins that are tumor free) and separating muscles that can be preserved and leaving those in continuity with the tumor that should be removed. This is based on preoperative MRI and intraoperative findings as well as the type of tumor.
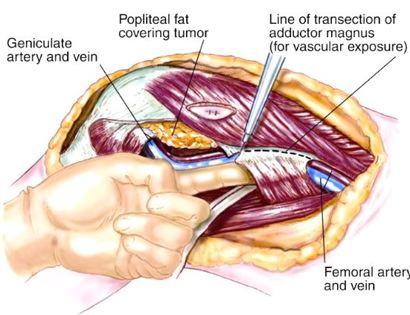
Blood Vessel and Nerve Dissection
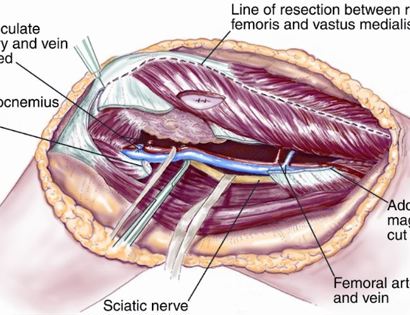
In rare cases a nerve (s) may need to be removed if it is involved by the bone sarcoma. For this procedure it is vital that the femoral vessels (femur artery and veins), popliteal vessels (arteries and veins around your knee joint), and sciatic nerve are properly identified. Once the blood vessels and nerves are properly identified they can be retracted (moved away) and protected throughout the procedure.
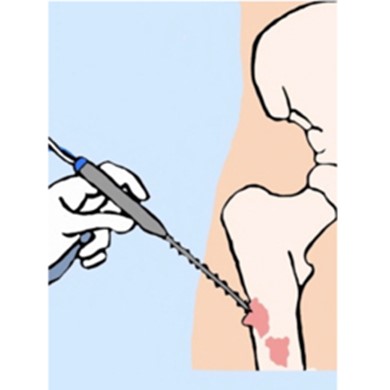
Tumor Removal with Surgical Saw
The femur bone is cut with a surgical saw, about 1 cm longer than the than the planned replacement. This is done to create the largest possible platform for the tibial component of the prosthesis.
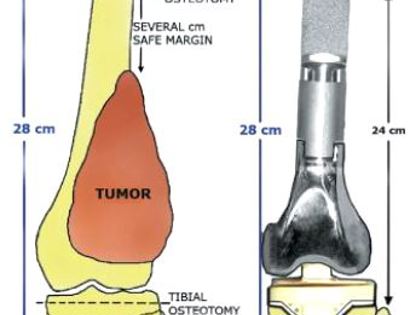
Tumor Removal and Reconstruction
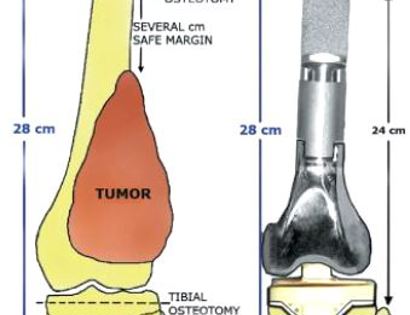
Removal of tumor and reconstruction with a tumor prosthesis. Reconstruction of the lower leg/knee utilizing a specialized tumor prosthesis is the most common limb-sparing technique for bone sarcomas, soft-tissue sarcomas, or large benign aggressive tumors that have destroyed the bone arising in this area. This prosthesis is sized and built during the surgical procedure then implanted and secured in place using cement. The length of bone removed is based on preoperative X-rays and MRI.
Distal Femur Reaming
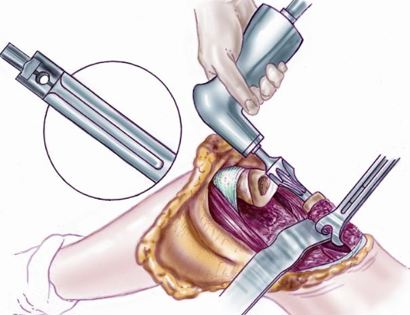
The inner bone is drilled into in order to fit the largest possible femur prosthesis.
Distal Femur Prosthesis Components 2

This femur prosthesis is sized and built during the surgical procedure then implanted. We cement the prosthesis into your bone and safely secure it in place.
Distal Femur Components Schematic
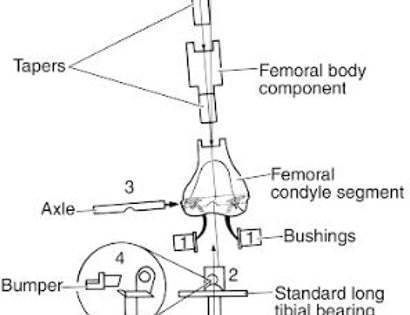
This is a diagram of how all of the parts of the femur prosthesis fit together
Distal femur Prosthesis Implanted
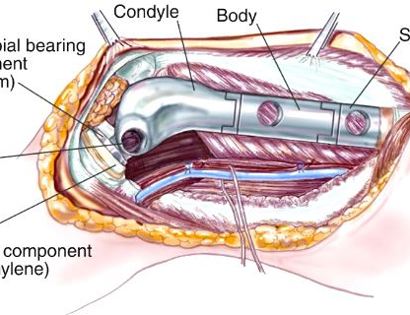
The prosthesis is measure to ensure the proper fit once inserted into the upper femur and connecting to the upper tibia.
Soft Tissue Coverage
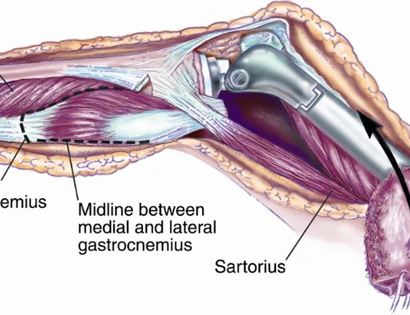
After the prosthesis is inserted local muscle is used to attach and cover it to ensure proper function post-surgically.
Soft Tissue Coverage
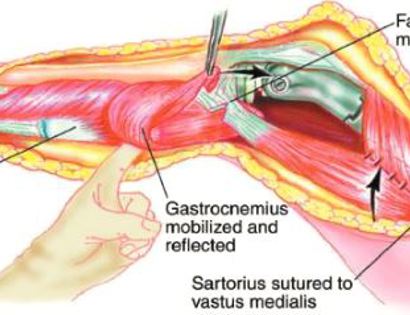
Soft tissue coverage of the prosthesis. Multiple muscle rotation flaps are used to restore function and stability of the knee as best as possible. The goal is to provide a stable knee so the extremity can function well. Soft-tissue reconstruction that involves rotating and reattaching the surrounding muscles, including the gastrocnemius (calf muscle) and vastus medialis (quadriceps muscle). Restoring the function of the surrounding muscles and knee joint is most important for achieving optimal functional outcomes and for protecting the prosthesis from infection.
Closure
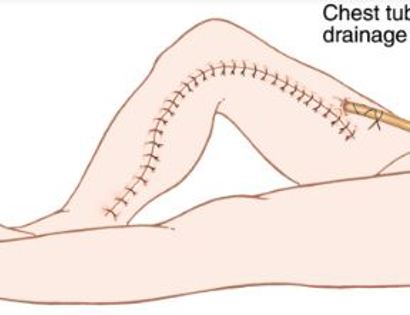
We then close your incision with sutures and cover the surgical site with bandages. Multiple large drains may also be used to drain the surgical site and prevent a seroma (buildup of fluid).
Distal Femur X-ray of Tumor

This is an x-ray image of the lower femur bone. The lighter area surrounding the bone is all tumor growth.
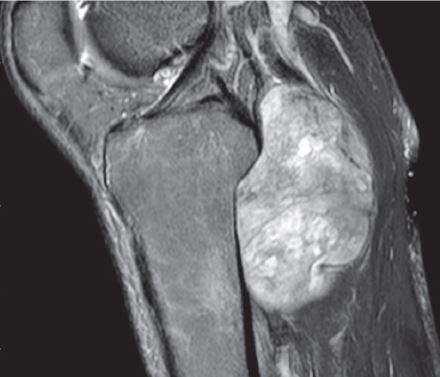
Distal Femur MRI of Tumor
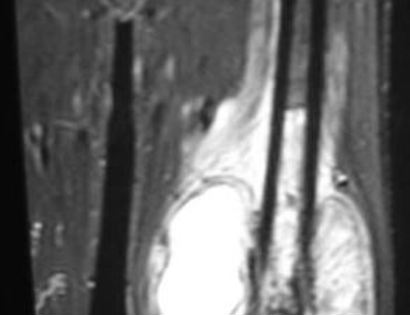
This is an image of the soft tissue component of a tumor growing on the lower left femur bone (right side of the image). The tumor is highlighted.
X-ray Photo

This is an x-ray of the patient post-operatively after the insertion of the prosthesis.
Intra-Op: Incision

The femur is marked for surgery with the incision being made ranging from the upper thigh to the upper calf. The previous biopsy is left intact as seen by the ellipse.
Intra-Op: Blood Vessel and Nerve Dissection
This is an image of the patient’s femur. The veins and major arteries are tagged with sutures to ensure that they are identified and protected.
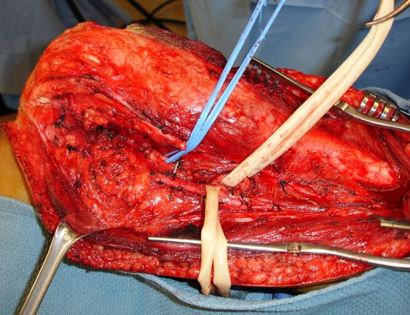
Intra-Op: Tumor Isolated

This is an image of the isolated tumor from the lower part of the femur bone.
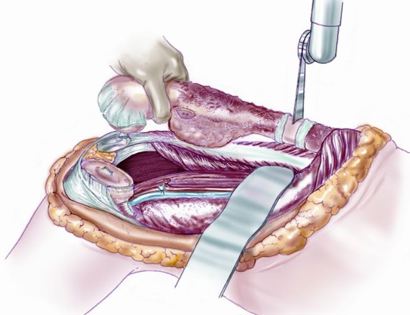
Intra-Op: Specimen Photo

This is an image of the tumor after being fully removed from the patient.
Intra-Op: Prosthesis Inserted

This is an image of the fitted prosthesis after being placed into the patient.
Intra-Op: Soft Tissue Coverage

After the prosthesis is inserted into the femur bone, muscle is used to attach and cover the prosthesis to ensure proper functioning post-surgically.
What you can expect afterwards
After your surgery you will spend a few nights in the hospital and then will be recuperating at home. Various pain protocols and nerve blocks are used to minimize pain. Mostly all patients are very comfortable after the surgery. For the first few days you will ice the area and keep it elevated to reduce swelling. You will return to the office 2 weeks after surgery. Patients are usually kept in a knee brace with the knee fully extended for 6 weeks to allow tendon and muscle to heal down to the prosthesis. This is important for the ultimate function of the prosthesis as the biggest difficulty after this surgery is extending the knee completely. After 6 weeks, the muscle and tendon should be healed down to the prosthesi sufficiently to start controlled knee flexion in the brace. You will then proceed to flex the knee 10-20 degrees per week in the brace. You will be advanced 10-20 degrees per week provided you can get your knee straight on your own in the brace. In addition, once cleared, you will subsequently start physical therapy. We usually prescribe specific physical therapy protocols 3 times a week for 12 weeks after surgery to gradually strengthen muscles. Strengthening with significant resistance after sufficient range of motion is achieved as determined by Dr. Wittig. There may be an ultimate weight limit imposed upon you depending on various factors.
You will be monitored periodically with X-rays over the course of 5 years. Sometimes an MRI and/or CT may be used to additionally monitor the area to make sure the tumor has not come back. You will then have follow up appointments every 4 months for the first 2 years, then every 6 months for the next 2 years, and then once a year. Since the bone integrity has been restored to full or almost full, recovery is anticipated provided the patient adheres to strict physical therapy.
Distal Femur Tumor Removal Video
Dr. James Wittig narrates a video illustrating the surgical technique for resection of a sarcoma of the distal femur and reconstruction utilizing a tumor prosthesis. | WATCH VIDEO